The Department of Orthopaedics is dedicated to cultivating clinicians and trainees who embody the principles of service, learning, and giving. This commitment is reflected in their global initiatives, which focus on building meaningful relationships, providing essential training for healthcare professionals in underserved countries, and developing innovative research and practice models. As faculty and staff continuously seek new opportunities to make an impact, the Department’s global programs are ever-evolving and expanding. They are engaged in various capacities across diverse locations, including Africa, France, Ghana, Honduras, India, New Zealand, San Salvador, Norway, Nepal, Jamaica, Kuwait, Sri Lanka, and Tanzania, working tirelessly to assist those in greatest need.
Ghana

A dedicated team of Duke Orthopaedics faculty members—Yaw Boachie-Adjei, MD, clinical associate of Orthopaedic Surgery; Co-Section Head, CDHIP; Tyler Pidgeon, MD, associate professor of Orthopaedic Surgery; and Dave Ruch, MD, Virginia Flowers Baker Distinguished Professor of Orthopaedic Surgery; Hand, Wrist, and Upper Extremity Division Chief—traveled to Accra, Ghana, to volunteer at The Foundation of Orthopaedics and Complex Spine (FOCOS) Orthopaedic Hospital. Their mission was to provide care and expertise, working alongside local surgeons and residents to perform complex upper extremity surgeries and exchange vital knowledge.
Dr. Yaw Boachie-Adjei shared, "Participating in this medical mission trip has profoundly impacted my outlook on my career as a surgeon. The experience of providing critical care to underserved communities abroad renewed my passion for medicine. It reminded me of the profound difference we, as medical practitioners, can make in people's lives. Witnessing patients' resilience and gratitude firsthand deepened my empathy and compassion. This has led to stronger connections with my patients back home.
Moreover, collaborating with international healthcare professionals expanded my skillset and exposed me to innovative approaches, enhancing my expertise. The ability to teach them also provided a good exchange of knowledge and skills. I hope to continue to do valuable work in the future."

One of the most impactful parts of Dr. Blake R. Boggess' international work has been his involvement with the “Ghana Make A Difference” (GMAD) program. GMAD operates a children’s home for children who have been rescued from trafficking on Lake Volta, orphans, and children with special medical needs who have been abandoned. Dr. Boggess has participated in medical missions twice a year through GMAD, providing medical care, ultrasound triage, and health education in rural clinics and hospitals. During these trips, he often treats over 200 patients daily as part of a multispecialty team, bringing much-needed medical services to communities that lack access to primary healthcare.
“It is always humbling to see the resilience and hope in the patients we care for,” says Dr. Boggess. “These missions are a reminder of the importance of healthcare as a basic human right and the difference that compassionate care can make.”
In addition to his work with GMAD, Dr. Boggess has significantly contributed to medical education in Ghana and Uganda. With Duke University's support, he has taught ultrasound to clinicians and medical staff, enhancing their ability to diagnose and treat various conditions. Additionally, he has facilitated the donation of surplus medical supplies and decommissioned equipment, such as ultrasound machines, which continue to support healthcare in these regions.
France

Dr. Chad Cook, PT, PhD, MBA, FAPTA, professor of Orthopaedic Surgery; director of Clinical Facilitation Research, Director of Duke Center of Excellence in Manual and Manipulative Therapy, is an experienced educator and speaker with over 10 years of delivering workshops and presenting at congresses across multiple cities in France. He has built solid and collaborative relationships with French physiotherapists, which have evolved to encompass many professional engagements, including online educational programs, research collaborations, and lasting personal connections. His dedication to advancing knowledge and fostering meaningful partnerships in the physiotherapy community has contributed to his reputation as a trusted and influential figure in the field.
Uganda

Dr. Blake Boggess traveled to Africa to direct a musculoskeletal ultrasound course in Kampala, Uganda. In October 2019, he had previously been the keynote speaker for the Orthopaedic Society of Uganda. He was invited back to direct a course for the orthopaedic society with the Association of Radiologists in Uganda.
Dr. Boggess was accompanied by his wife, Amelia, two additional physicians, three physiotherapists, one sports scientist, and two university student assistants. The team organized and taught a two-day sports medicine/ physical therapy symposium at Mbarra University of Science and Technology. They wrapped up their medical mission by evaluating and treating the Ugandan National Athletics team in preparation for the Pan African Games.
Blake has directed over 38 ultrasound courses, including Russian, China, Cuba, Ghana, and Taiwan.
New Zealand
Chad Cook, PT, PhD, FAPTA, a professor in the Division of Physical Therapy, was awarded the prestigious University of Otago Stanley Paris Traveling Research Fellowship in 2024. During his trip in March, Dr. Cook engaged in collaborative discussions with Dr. Nadine Foster from Australia and conducted several workshops at the University of Otago in Dunedin. Additionally, he had the opportunity to explore New Zealand's South Island alongside Dr. Stanley Paris, the benefactor of the fellowship and the visionary donor behind the establishment of the Duke Center of Excellence in Manual and Manipulative Therapy. This experience enhanced Dr. Cook's research and teaching initiatives and strengthened international ties in physical therapy.

Vietnam
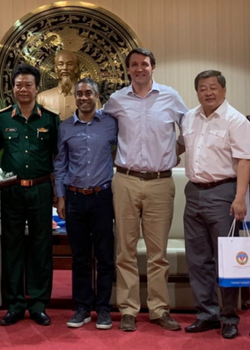
Duke Orthopaedic hand surgeon Dr. Marc Richard joined a group from Stanford University for a visit to Hospital 175 in Ho Chi Minh City, Vietnam, for a week-long exchange, including education, surgery, and the establishment of research protocols to understand the effect of the mission trip.
The Stanford team members included Dr. Robin Kamal (Duke Hand Fellowship alumnus) and Dr. Lauren Shapiro (Duke Hand Fellowship alumna). Preparing to treat patients who traveled from all over Vietnam, the team spent their first day in the indications clinic, where they examined varied and complex cases. Subsequently, the next few days were spent in the operating rooms in the mornings and teaching, lecturing, and reviewing case presentations in the afternoons. The team primarily performed hand and upper extremity cases, including distal radius fractures, both bone forearm fractures, distal humerus and humeral shaft fractures and malunions, distal radius mass biopsy, elbow instability, and multiple tendon transfers for a patient with a radial nerve injury following a motorbike accident.
Through a grant, the group established follow-up protocols for operative patients through a smartphone text message system, including the use of patient-reported outcome measures. The goal is to understand the ability to affect change through episodic mission trips and to identify barriers to success so that necessary changes can be made.
Australia

The legacy of critical illness leaves millions of survivors worldwide with long-lasting deficits in physical and brain function as well as anxiety, depression, and post-traumatic stress disorder. Early rehabilitation in the intensive care unit (ICU) may prevent or minimize these effects. Amy M. Pastva, PT, MA, PhD, is collaborating with a global team from the University of Melbourne/Austin Health, Australia (Sue Berney, PT Ph.D., and Linda Denehy, PT, Ph.D.), Royal Brisbane and Women’s Hospital, Australia (Jennifer Paratz, PT, Ph.D.), and Johns Hopkins University, USA (Dale Needham, MD, Ph.D.), to study the effectiveness of functional electrical stimulation of leg muscles during in-bed cycling (eStimCycle) on muscle bulk, strength, physical function and brain function at hospital discharge and at 6 and 12 months afterward in patients who were critically ill in the ICU (ClinicalTrials.gov ID: NCT02214823). This is one of the first of global studies in critical care rehabilitation and the combined effort will help guide treatment strategies worldwide for patients at high-risk for ICU-acquired deficits.
El Salvador
Former Duke residents and fellows, including Dr. Daniel Mangiapani, Dr. Jordan Schaeffer, and Dr. Tim Randell, traveled to San Salvador to participate in Operation Walk Utah. Operation Walk Utah was started in 2007 by Dr. Aaron Hofmann (Hofmann Arthritis Institute), who dreamed of doing free surgeries in third-world countries with a team of volunteers. It is a private, not-for-profit, volunteer medical service organization that provides free joint replacement surgeries for patients with disabling arthritis in developing countries and in the United States. Operation Walk also educates in-country orthopedic surgeons, physical therapists, and other healthcare professionals about advanced treatments and surgical techniques for diseases of the hip and knee joints.
During the trip to San Salvador, the Operation Walk Utah team performed 72 joint replacements in 5 operative days, spanning 3 ORs. Cases ranged from a 35-degree valgus knee with MCL incompetency to bilateral total hip arthroplasty on severely dysplastic hips. On the team’s final day, they rounded on all the inpatients, whose joy and happiness radiated on their faces and their families' faces.
“It was, no doubt, a life-changing experience that has changed my outlook on what ‘service’ truly is,” says Dr. Mangiapani.