Healthcare faces growing challenges—rising costs, variable quality, and increasing provider burnout. Musculoskeletal conditions are a major contributor to this burden, impacting patients, providers, and health systems both locally and nationally.
To lead change, the Practice Transformation Unit (PTU) was launched within the Duke Department of Orthopaedic Surgery. The PTU actively reimagines how orthopaedic care is delivered, experienced, and financed.
Our mission is clear: to elevate the value of musculoskeletal care. We design, test, and scale innovative care and payment models that improve outcomes, reduce costs, and enhance the experience for both patients and providers. Through collaboration and data-driven strategies, the PTU is shaping a more sustainable and equitable future for orthopaedic healthcare.
PTU Team
Strategy
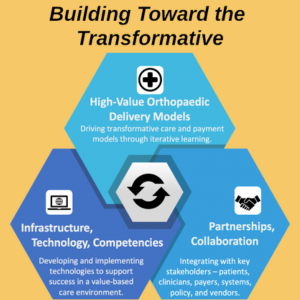
Espousing a bias toward action, the PTU is quickly and relentlessly enacting its strategy. Whereas many attempts at healthcare solutions address a single isolated dimension (e.g., technology, policy, care delivery), the PTU pursues an integrated approach. It recognizes the power of architecting infrastructure and crafting policies that enable transformative care models in which clinicians enjoy practicing, which, in turn, feed back iteratively to inform smart infrastructure investments and focused, pragmatic policies.
Development
Care Model
The Duke Joint Health Program (JHP) care model addresses the sizable gaps and opportunities in the comprehensive care of hip and knee osteoarthritis through a longitudinal, adaptive, personalized lifestyle and behavioral health modification program coordinated and managed by multidisciplinary Primary Osteoarthritis Providers (POPs), who are physical therapists trained in cognitive-behavioral theory-based strategies.
Partnerships
Healthcare payment reform. Recognizing the crucial need for new ways to pay for new care models, the PTU is deepening its productive working relationship with the Duke-Margolis Center for Health Policy and engaging local and national payers, health systems, policy groups, and others in the design and implementation of condition-based (as opposed to episode-based or fee-for-service) payment models to improve the musculoskeletal health of affected populations.
Duke Doctor of Physical Therapy and Duke Occupational Therapy Doctorate programs. Using the deep collaboration and teamwork fostered between orthopaedic surgeons and physical therapists to launch and maintain the Joint Health Program care model is a joy. Effectively caring for patients with chronic musculoskeletal conditions takes a team of appropriately skilled multidisciplinary providers who deliver the right care at the appropriate times and in the right settings.
Infrastructure and Technology: As detailed below, the PTU's progress would not have been possible without deep and broad collaboration with various entities in the healthcare sphere.
Infrastructure
Orthopaedic data universe. Working with the Comprehensive Outcomes in Orthopaedics and Rehabilitation Data System (COORDS), Duke Health Technology Solutions (DHTS), and the Analytic Center of Excellence (ACE), the PTU is helping to develop an accessible clinical data-collection system. Through COORDS, Duke Orthopaedics has also collected baseline PROMIS data on tens of thousands of patients across all orthopaedic divisions and hundreds of providers.
Intelligent ambulatory clinic scheduling. Working with Apprentice Health, the PTU is implementing orthopaedic ambulatory scheduling changes to reduce unnecessary wait times and drive down cycle times. This is done through a combination of provider clinic-day preferences, deep learning simulations, and objective patient flow data captured through a passive low-energy Bluetooth tracking system.
No-show predictor model. Working with Jvion, Duke Orthopaedics is testing a no-show predictor model in its clinics that identifies patients at high risk of no-shows or late cancellations using more than 4,000 different factors for analysis.
Telehealth visits. Working with the Duke Telehealth Office, the PTU established telehealth visit centers at two orthopaedic clinic locations. Patient experience metrics reflect positively on the use of telehealth in an orthopaedic setting.
Machine learning applications for knee osteoarthritis. Collaborating with the Duke Department of Radiology and the Forge, the PTU is developing a machine-learning algorithm to automatically grade the severity of knee osteoarthritis on radiographs as part of a larger project applying acceptable use criteria for total joint arthroplasty.
Personalized digital care platform. The PTU is working with Xealth and Pattern Health to implement a connected-care digital health platform to deliver personalized, condition-based care pathways to patients in the Joint Health Program and those undergoing other orthopaedic surgical and non-surgical treatments.
Contact
For inquiries regarding the Practice Transformation Unit, please contact Bill Jiranek.